Researchers from the University of Cambridge, University of Oxford, and The Pirbright Institute have discovered how poxviruses evade natural defences in living cells and realised that drugs to stop them doing this are already available.
Published in Nature, this research has investigated how poxviruses overcome human cell defences and from this have identified a potentially more resilient treatment strategy. Scientists have uncovered how poxviruses exploit a cellular protein to outwit host defences, enabling efficient replication and transmission.
Current drugs designed for immunosuppression or other viral infections target this protein. The researchers noted these drugs also impede poxvirus replication and spread. Unlike conventional antivirals, which target a virus protein, this method targets a cellular protein so making it challenging for the virus to develop drug resistance.
Given the shared hijacking mechanism among various poxviruses, this approach holds promise in treating multiple diseases, including mpox and smallpox. Whilst these are looking at human poxviruses other poxviruses affect animals and can be fatal, including lumpy skin disease and sheep and goatpox virus.
The containment level 3 (CL3) facilities at Pirbright enabled Professor Geoffrey L. Smith, and Drs Yongxu Lu and Yiqi Zhao from the University of Cambridge to undertake the research on monkeypox virus.
This collaboration demonstrates the importance of fostering relations and groups such as the recently formed Monkeypox Consortium. It also highlights Pirbright’s capability and robust laboratory infrastructure which offers scientists the ideal platform to advance their research, reinforcing a comprehensive ‘one health’ strategy towards managing epidemics.
With the capacity to contribute significantly to outbreak situations, Pirbright's capabilities focus largely on livestock viruses but will extend to assist both domestic and global public health responses. By facilitating collaborative research such as this project, the Institute plays a pivotal role in enhancing our understanding of epidemics and fortifying public health measures, both within the UK and on an international scale.
Professor Geoffrey L. Smith, who conducted the work in the Department of Pathology at the University of Cambridge, the Dunn School of Pathology, University of Oxford and at Pirbright, said, “The drugs we identified may be more durable than the current treatment for monkeypox – and we expect will also be effective against a range of other poxviruses including the one that causes smallpox.
Once a poxvirus infects a host cell, it has to defend itself from attack by cellular proteins that would restrict virus replication and spread. Researchers identified a specific cell protein, called TRIM5α that restricts virus growth – and another cellular protein called cyclophilin A that prevents TRIM5α doing so. Existing drugs target cyclophilin A, and so make the virus more sensitive to TRIM5α.
“There are various drugs that target cyclophilin A, and because many of them have gone through clinical trials we wouldn’t be starting from scratch but repurposing existing drugs, which is much quicker.
“Our results were completely unexpected. We started the research because we’re interested in understanding the basic science of how poxviruses evade host defences and we had absolutely no idea this might lead to drugs to treat monkeypox virus and other poxviruses.”
Professor Guy Poppy, Interim Executive Chair at the Biotechnology and Biological Sciences Research Council (BBSRC), said: “The national monkeypox consortium was borne out of an urgent need for the UK to respond to an emerging threat of disease caused by this virus. It is critical that public funders and policy makers are able to act with agility and coordination to support a swift scientific response.
“Taking a One Health approach, the rapid response by BBSRC and the Medical Research Council (MRC), in collaboration with policy makers via the UKRI Tackling Infections strategic theme, enabled leading researchers from across the UK to pool their expertise and deliver impactive results at pace.”
For further information on the research project, see the University of Cambridge website.
The research was funded by the Department of Pathology, University of Cambridge, The Isaac Newton Trust, MRC, Wellcome and a UKRI BBSRC consortium grant awarded in 2022 in response to the mpox outbreak.
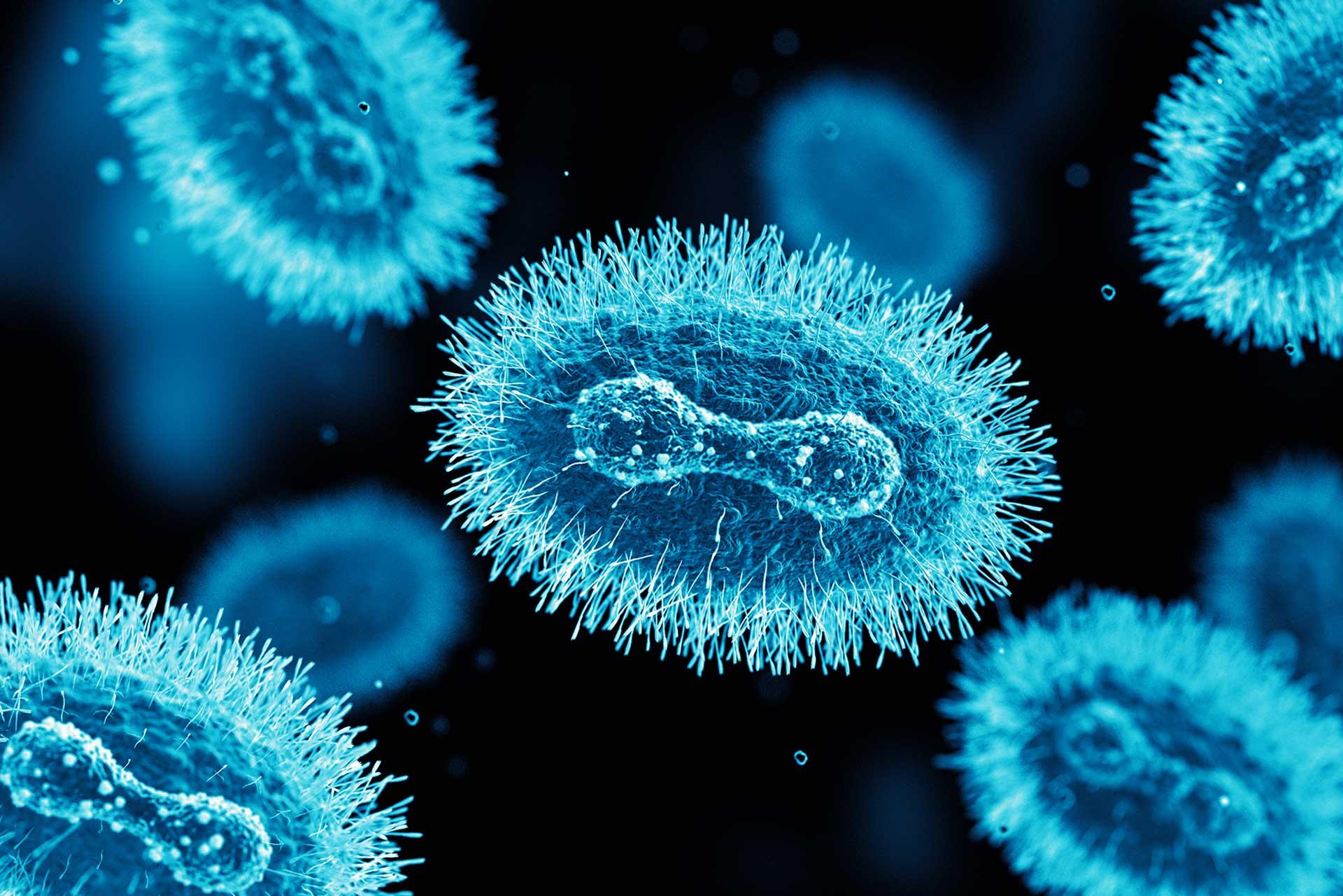
Image caption: Monkeypox virus under the microscope. Credit: BlackJack3D.