Experiments by researchers at The Pirbright Institute have identified the molecular mechanisms that enable H9N2 viruses - the most common type of avian influenza (bird flu) virus - to infect humans, helping improve risk assessments for its potential to cause pandemic.
Although H9N2 viruses are considered less pathogenic than some types of avian influenza virus, they still cause significant losses for the poultry industry in many countries throughout Asia, the Middle East and North Africa – sometimes with death rates as high as 60%.
Over the past 20 years there have also been a growing number of (generally mild) human infections of H9N2 in Hong Kong, mainland China, Bangladesh and Egypt, especially amongst poultry workers. Concerns increased however when other experiments demonstrated the potential for human-to-human airborne transmission; a property normally associated with the potential to cause pandemic.
Despite the widespread global distribution and diversity of H9N2 viruses and their potential threat to human health, they have not been extensively characterised until now. In new research undertaken by Pirbright scientists and published in the science journal Nature’s Emerging Microbes & Infections, researchers analysed the specific properties that enable some lineages of H9N2 to adapt for successful human infection.
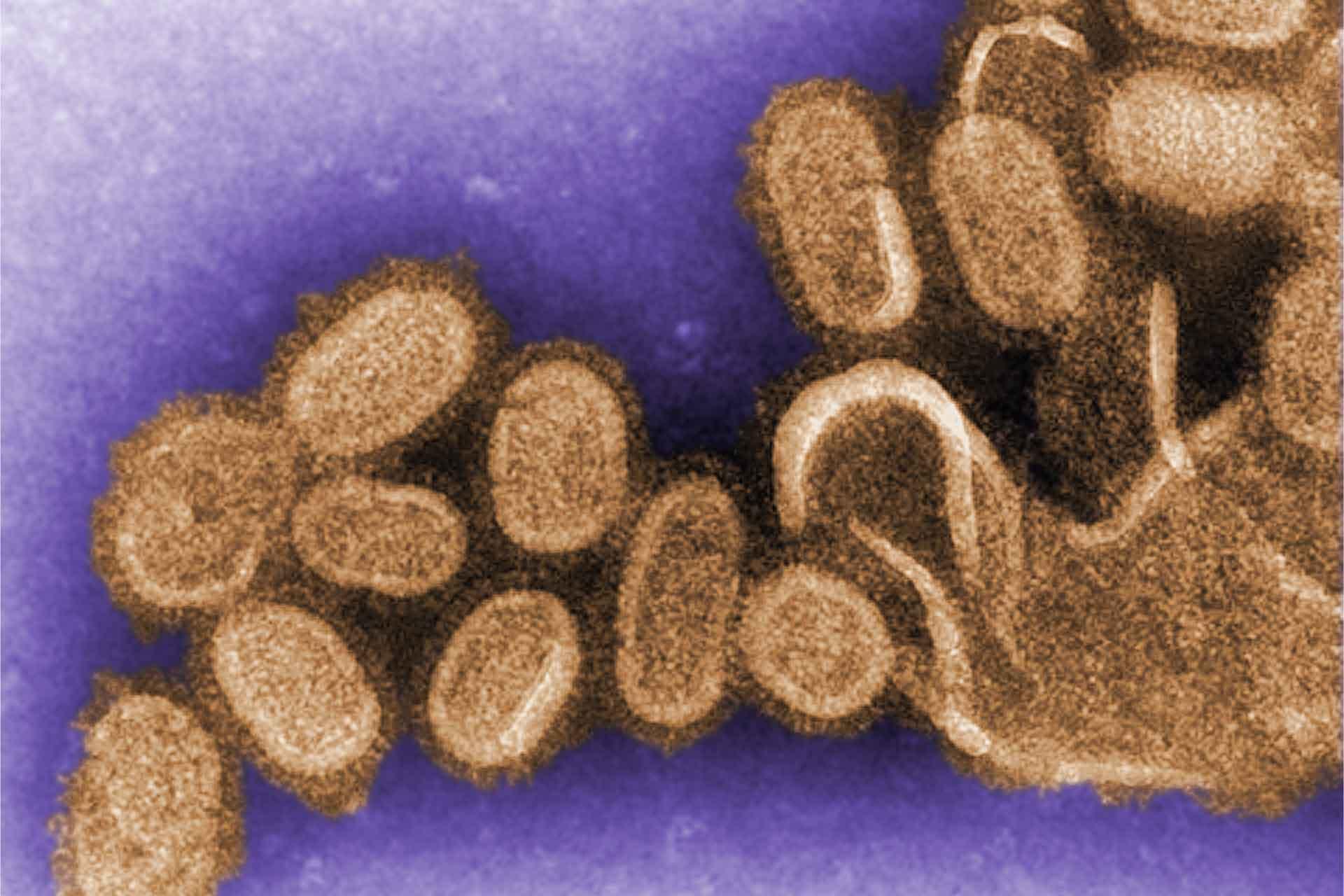
Led by Dr Munir Iqbal, head of the avian influenza virus group at Pirbright, researchers specifically focussed on the surface protein haemagglutinin, which enables the virus to bind and fuse with host cells for entry and infection. In particular scientists investigated two properties that facilitate adaption for human infection: its preference for binding to different host receptors (molecules on the surface of a cell responsible for communication) that allow cell entry and the pH level at which the virus can fuse with the host cells (pH of fusion) and therefore begin infection.
Dr Iqbal’s team aimed to explore the potential relevance of these biomarkers for zoonotic (disease capable of spreading from animals to humans) risk assessments. They characterised which host cell receptors the H9N2 haemagglutinin prefers to bind to, which is important as human and bird receptors are slightly different, which usually means that bird flu strains bind to ‘bird-like’ receptors and human strains bind to ‘human-like’ receptors. Bird flu strains can infect humans when a mutation occurs that enables a preference for binding receptors that are ‘human-like’. This has been partially or entirely attributed to a single amino-acid change in the haemagglutinin.
The team also assessed how the stability of H9N2 haemagglutinins affects the pH of fusion. In order to infect humans, the haemagglutinin must be stable enough to survive in respiratory droplets for airborne transmission and in the mammalian nasal tract, which is mildly acidic (less than a pH of 7). Haemaggluttinins of human flu strains have adapted to be stable and fuse at an acidic pH that is typically less than 5.5, whereas avian flu strain haemagglutinins are generally more stable above this level and are therefore unable to fuse in the acidic conditions of the human nasal tract.
The H9N2 strains being investigated were found to possess haemagglutinins which were stable at lower pH levels, something which was mirrored in other bird flu strains which have adapted to infect humans in the past. It was established that the stability at a lower pH was a more important factor for virus fusion than the preference for binding to different receptors.
Dr Iqbal said: “Based on the two properties we tested, our results indicate that the lineages with the highest zoonotic potential may be those currently circulating in southern China and Vietnam (G1 ‘Eastern’ sub-lineage). However, evaluations in this study of the lineages prevalent in China and Vietnam (BJ94) and from Bangladesh to Morocco (‘Western’ G1 sub-lineage), suggest these viruses could also adapt to humans with relatively few additional mutations and merit further research.
“This study has provided us with some important new insights which are helping us develop our understanding of these influenza viruses from molecular, biophysical and virological perspectives. We hope this will inform risk assessments of their zoonotic and pandemic potential and help improve global vaccine strategies”.
This research was funded by The Pirbright Institute studentship grant, Biotechnology and Biological Sciences Research Council (BBSRC) ZELS grant and the BBSRC Avian Disease Programme grant. Work at the World Health Organization (WHO) Collaborating Centre in London was supported by the Francis Crick Institute, which receives its core funding from Cancer Research UK, the Medical Research Council and the Wellcome Trust.
*Image courtesy of Cynthia Goldsmith from the Public Health Image Library