Understanding how cell memory is induced and maintained helps scientists to study immunity and design more effective, long-lasting vaccines.
In a collaborative study, researchers from The Pirbright Institute, the Institute for Infection & Immunity, City St George’s, University of London and Imperial College London sought to investigate how memory cells in tissues such as the lung are maintained in situ and establish whether cellular longevity or cell division and replacement drives immunity.
The researchers chose to study the pig lung since the pig respiratory tract has many anatomical and physiological similarities to humans and the pig is a natural host for similar influenza A viruses to those found in humans.
To address the rate of division of lung tissue resident memory T cells (TRM), deuterium-enriched water was administered orally to young pigs to label dividing lymphocytes in a study involving 13 animals.
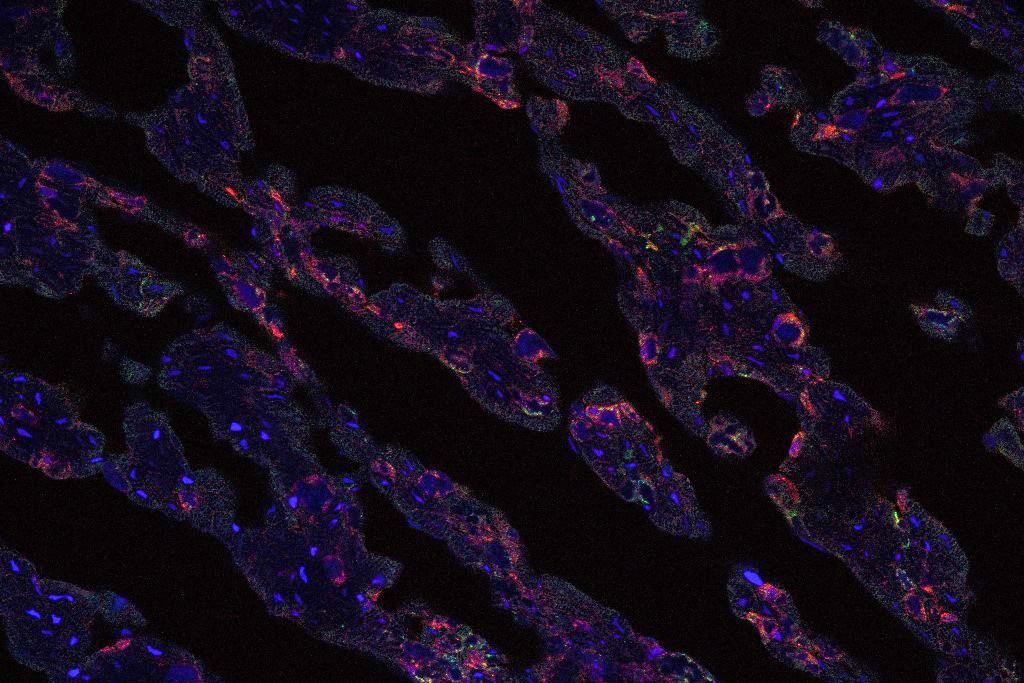
T cell subsets were separated from blood, lymph nodes and airways (bronchoalveolar lavage, or BAL), the latter comprising almost exclusively TRM.
“Our data excluded long-lived TRM cells in BAL and gave us three possible hypotheses: blood/airway exchange, in situ proliferation, or proliferation in the lung interstitium followed by migration to BAL,” said Prof. Elma Tchilian, Head of Mucosal Immunology at Pirbright,
The lung interstitium contains connective tissue and is the space between the air sacs and the small blood vessels that surround the sacs.
“We favour the latter interpretation. Our study fits a model in which airway TRM are non-dividing in situ but are replenished from a lung interstitial TRM population with a similar T cell receptor repertoire, dividing at a similar rate to circulating blood and lymph node cells.”
The research confirmed that circulating naïve cells divide more slowly than memory T cells and indicated that airway TRM are actively replenished by cell division at a substantial rate, highlighting the dynamic nature of memory in the lung with implications for harnessing immune responses against respiratory pathogens.
“Our experiments have established a novel methodology for studying cellular kinetics in a large animal with many similarities to humans. Our results indicate, that irrespective of the mechanism, TRM are derived from cells which divide at a similar rate to analogous memory phenotype cells in blood or lymph node,” said Prof. Derek Macallan, Principal Investigator in the Infection and Immunity Research Institute, School of Health and Medical Sciences, City St George’s, University of London, and practising clinician in Infectious Diseases at St George's Hospital.
The expanding toolkit for studying porcine immune responses, coupled with advances in annotating the porcine genome and the application of scRNA sequence (scRNA-seq) analysis, has significantly enhanced the utility of the pig as a biomedical model.
All experiments were approved by the ethical review processes at The Pirbright Institute and Animal and Plant Health Agency (APHA) conducted according to the U.K. Government Animal (Scientific Procedures) Act 1986 supported by a Project License.
Read the paper
Vatzia, E., Zhang, Y., Sedhagat-Rostami, E., et al. (2025) Proliferation makes a substantive contribution to the maintenance of airway resident memory T cell subsets (TRM) in young pigs. Discovery Immunology https://doi.org/10.1093/discim/kyaf007